Episode 48: Let’s Talk About Food Insecurity and Health at Every Size

About the Podcast
Kimmie Singh is a Registered Dietitian based in New York City. In this episode, she calls on health professionals to acknowledge food insecurity, among other lifestyle factors, to treat the whole patient. She tells all, from her secrets for treating eating disorders to outlining the basics of the Health at Every Size approach.
About Kimmie Singh
Kimmie Singh is a fat Registered Dietitian based in New York City. She completed her Bachelor of Science in Physics from St. John’s University, her Master of Science in Nutrition at The University of North Carolina at Greensboro, and her Dietetic Internship from The City University of New York-Hunter College. Kimmie is an associate at LK Nutrition, a Health at Every Size private practice that supports clients with eating disorders and disordered eating heal their relationships with food and body. She specializes in providing support for PCOS management. She also presents and consults on weight stigma in healthcare. Kimmie is a believer in kindness, compassion, and the power of advocacy.
Discussion Takeaways
- Kimmie’s eating disorder recovery motivated her to become dietitian to help guide others through the process.
- Being food insecure may mean you have more than enough of a certain type of affordable food, instant noodles for example, but you might not have access to the variety of foods you need to stay healthy.
- Often, people without money do not have the privilege to explore their relationship with food. There is psychological stress and shame that comes with poverty. Too, socio-economic barriers limit regular access to nourishing foods. It’s a really complicated issue.
- Parents will often hide the fact that they don’t have enough money for food. But, kids can see through this façade, even though they weren’t explicitly told about it. By not giving space to talk about their struggles, parents are not allowing kids to process the reality of their situation, the feeling of being hungry regularly, and its impact on their relationship with food in the future.
- By calling someone “overweight” and “obese” or using the Body Mass Index (BMI), you are pathologizing or treating their bodies as abnormal or unhealthy. Many health professionals are now asking their patients about how they would classify their own body type. Too, they turn toward terms like “larger bodied”, “heavier bodied”, or “fat”.
- Kimmie self-identifies as “fat”. There is beauty in neutralizing this word and ridding of the stigma behind it.
- When presenting, health professionals can refer to studies that describe bodies by using BMI over a certain number. Then, you can specify that this terminology is used only within the study. Throughout the rest of your presentation, you can use the less offensive terms stated above.
- Suffering from food insecurity and utilizing federal food assistance often causes people to get caught in a cycle: having enough money for food at the beginning of the month and starving toward the end of the month when their federal benefits run out. People separate from their satiety cues when they don’t have enough funds for a well-rounded diet. It only makes sense that when they can afford food, they still struggle to balance their hunger and fullness. This disconnect causes people to struggle with self-regulation surrounding their food choices. And when someone has the money, they want a sense of normalcy and buy celebratory foods often in excess.

- The Health at Every Size (HAES) doesn’t mean every body is healthy at various sizes, whether large or small. This philosophy is about encouraging health-promoting behaviors regardless of someone’s body size, rather than prioritizing weight loss. HAES is based on five main principles: 1) weight inclusivity, 2) health enhancement, 3) offering respectful medical care, 4) eating for wellbeing, and 5) joyful movement.
- Food, nutrition educators and healthcare providers can't assume anything. They also should recognize their immediate biases. Recipes, resources, and nutrition education programming should always center the clients' wants, needs, capabilities, and circumstances.
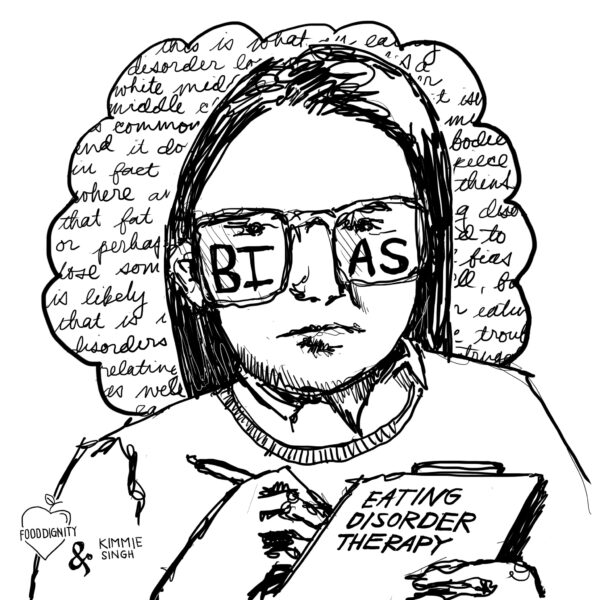
The beautiful images above were created by Rebecca Garofano, our Food Dignity Institute Lead and Illustration Specialist. You can find more of her work at @VeggieDoodleSoup on Instagram and at her website veggiedoodlesoup.com.
#1 tip to improve access to healthy food
People can maintain a scarcity mindset around certain foods. When benefits or money are limited, people might not give themselves permission to eat these foods. When these items become more accessible, people often have issues with self-regulation and could overindulge. This cycle is seen in those who suffer from food insecurity, eating disorders, or both.

Each week on the Food Dignity® Podcast, the Food Dignity® Movement’s Clancy Harrison hosts a wide variety of hunger experts and other people making changes on the frontlines. Join us as we dive deep into conversations that will change the way you think about food insecurity.
Listen to our trailer!
Want to learn more about how we might work together?

Fight hidden hunger by becoming a
Food Dignity® Champion and take the HIDDEN HUNGER PLEDGE >


